Treated Conditions
Type 2 Diabetes
Type 2 diabetes is a common condition that causes the level of sugar (glucose) in the blood to become too high
Obesity
Obesity is a common disease involving an excessive amount of body fat
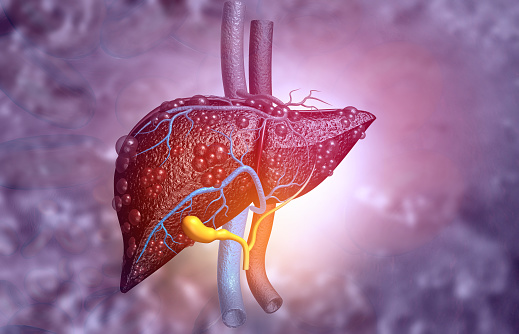
Fatty Liver Diseases
Fatty liver disease describes a range of conditions, including NAFLD and NASH caused by a build-up of fat in the liver